
Arthritis and osteoarthritis are complex diseases that affect the joints. Due to similar symptoms, many people think that these diseases are identical, but they are not. Arthritis and arthrosis differ in the causes of the disease, the nature of its development, the area of the injury, and require completely different treatment.
Suppose two people see a doctor complaining of joint pain. One was diagnosed with arthritis and the other with osteoarthritis. As both patients sat in line, they had time to discuss their health issues a bit.
It turned out that his symptoms are very similar: the joints hurt, they do not bend / unbend with all their strength, they do not give rest either at night or during the day. Even the diagnoses are consonant, but they are still different. What is the difference between arthritis and osteoarthritis if both diseases affect the joints?
What is arthritis
Arthritis is an inflammatory disorder of the joint. It is always preceded by some factor of damage to bone or cartilage tissue.
The destroyed cells release biologically active substances that trigger an inflammatory reaction. The vessels of the injury expand, fill with blood - due to this, immune cells go out into the joint tissue to fight the harmful factor.
At the same time, the liquid part of the blood leaves the vascular bed and an edema forms that limits the area of inflammation. This is how the body protects itself from extensive damage by bacteria, foreign bodies, and chemicals.
After total or partial elimination of the pathogen, the healing mechanism begins. If the damage was minor, normal tissue function will be restored. Deep defects heal through a scar, an area of rough connective tissue that does not perform the normal function of an organ.
Arthritis goes through all these stages:
- alteration - damage;
- exudation - the formation of edema;
- proliferation - healing.
Reasons
The causes of the disease are great, we will list the main ones:
- Streptococcal infection (tonsillitis, scarlet fever) often leads to a complication - rheumatism;
- aggressive autoantibodies: proteins that the body produces to fight its own tissues; such a situation develops with an error in the immune defense, which is why the joints are perceived as a foreign element to the body - rheumatoid arthritis;
- violation of purine metabolism leads to the deposition of uric acid crystals in the joints - gout;
- allergic reactions can involve joint tissue with the development of an inflammatory reaction - allergic arthritis;
- long-term use of certain medications causes inflammation (isoniazid, D-penicillins, hydralazine, holes): arthritis from medications;
- bacteria are carried in the bloodstream or during surgery: infectious arthritis;
- a viral or bacterial infection of any location can indirectly affect joint tissues; This is reactive arthritis;
- acute trauma: recent damage (impact, bruise, capsule rupture).

Symptoms
The disease is characterized by an acute initial stage, that is, against the background of full health, a person has acute pain in the joint. For autoimmune forms, symmetrical damage to small joints is characteristic: interphalangeal in the fingers, wrist, and elbow.
Gout in the vast majority of cases begins with inflammation of the joint between the thumb and foot. In bacterial and reactive arthritis, the large joints are usually affected on one side: the knee, the hip, the sacrum (at the junction of the spine with the pelvic bones).
Rheumatism develops against a background of fever and general weakness, usually preceded by angina. Severe inflammation of the bones, cartilage and synovium may occur with fever, general intoxication - headache, weakness, lack of appetite.
The skin over the joint becomes red and feels warmer than in other areas. Outwardly, it looks puffy and increases in volume. If the injury occurred on only one side, the difference between a healthy limb and a diseased one is visible.
Restricted movement is associated with swelling and pain. If the joint cavity is slightly inflamed, then it works almost completely. With a pronounced pathological reaction, the entire synovial cavity can fill with fluid; in this case, mobility is very limited.
Treatment
Treatment is performed by a general practitioner, rheumatologist or orthopedic surgeon, if the cause is mechanical damage. The therapy aims to remove the provoking factor and stop the inflammation.
For bacterial and reactive arthritis, antibiotics are needed, for autoimmune - cytostatics or glucocorticoids, for allergy sufferers - glucocorticoids and antihistamines.
Inflammatory fluid is withdrawn with a syringe or special suction during arthroscopy. The joint is immobilized for the entire period of acute inflammation. The patient is then shown therapeutic exercises to restore mobility to the joint.
Medical advice
From personal practice and work experience of colleagues - with joint inflammation of any etiology, gelatin compresses have proven themselves well. They are easy to implement and inexpensive. It is necessary to fold the gauze in several layers, the length and width should be such that there is enough for the sore joint. Dip the folded gauze in hot water, squeeze, straighten. Pour a thin layer of gelatin on top, roll it up so that it stays inside, like in a bag, and doesn't spill. Place on the joint, wrap with a polyethylene bag on top, fix with a bandage and / or adhesive tape. You can use a compress for up to 3 hours, 2 times a day for 2 weeks. Usually the effect is felt on day 4-5 of use, but therapy must be continued to achieve the desired result, if the course is interrupted, the pain will return.
What is osteoarthritis
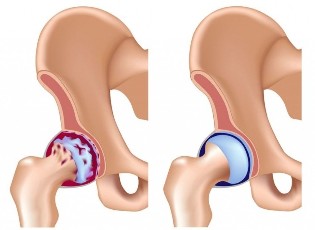
Osteoarthritis (otherwise osteoarthritis) is a degenerative-dystrophic disease. It is based on a deterioration in the nutrition of the articular cartilage, a slowdown in its recovery and a gradual loss of weight.
Simply put, the cartilage layer wears out faster than it rebuilds. The bony articular surfaces are exposed. They are not as smooth as cartilage and rub against each other with effort when moving. The bony plates are partially destroyed and mild chronic inflammation develops.
As the disease progresses, bone spines grow in the joint, a response of the protective tissue to permanent damage. They interfere with the sliding of surfaces against each other and the mobility of the joint is affected.
Osteoarthritis in most people begins to progress after 30-40 years, lasts for years, its symptoms are mild or moderate.
Osteoarthritis of the vertebral joints is often called osteochondrosis.
Reasons
There are predisposing factors that provoke the development of the pathology at an early age and complicate its course:
- intense physical activity among athletes;
- obesity;
- history of joint injury;
- vascular disease;
- sedentary lifestyle;
- violation of the normal configuration of the joint, for example, with flat feet;
- prolonged exposure to vibrations;
- in women: hormonal imbalance or menopause.
Symptoms
Large joints on one side are often affected: knee, hip, sacrum. The disease begins imperceptibly. Pain is rare at first and is associated with significant physical exertion.
The unpleasant sensations disappear the same day or in a few days if the person can rest. As the disease progresses, the intensity of pain increases, it occurs even with normal daily stress.
The mobility of the joint gradually decreases and as a result of the disease is completely lost. Movements in the diseased limb cause severe pain. Osteoarthritis can be aggravated by the type of arthritis: fluid accumulates in the joint cavity, the skin above becomes red and warm. Once the inflammatory reaction subsides, the course of the disease returns to its previous course.
Treatment
Osteoarthritis is treated by a traumatologist, an orthopedist, sometimes a surgeon. The therapy aims to restore metabolic processes in cartilage, improve joint nutrition, and eliminate the inflammatory response. Treatment is for life, it can be continuous or in drug cycles.
In the interictal period, chondroprotectors are prescribed in the form of tablets and ointments, therapeutic exercises, massage. With an exacerbation, chondroprotectors are administered intravenously or intramuscularly along with pain relievers and anti-inflammatory drugs. A trauma surgeon can inject protective medications directly into the joint every few months.
Advanced stages of the disease require surgical intervention, during which the diseased joint is replaced with an artificial one.
Differences between diseases
| Feature | Arthritis | Osteoarthritis |
| Cause of disease | Inflammation | Cartilage degeneration |
| Flow | Acute, chronic with exacerbations | Chronic |
| Pain | Intense from the beginning, more pronounced in the morning | At the beginning of the disease, weak, gradually increasing. It intensifies at night and after exertion |
| Movements | It is necessary to "spread out" - in the morning after sleeping the joints are the least mobile | Mobility gradually decreases, without morning stiffness |
| Affected joints | The small joints of the hands and feet are affected symmetrically. The big ones suffer from bacterial infection. | One or more large joints on different sides of the body |
| Blood test | Severe inflammatory changes in general blood test, rheumatoid factor, C-reactive protein, antibodies to pathogens | No typical changes |
| X-rays | Staged changes, osteoporosis: bone loss, bone cysts | Gradual changes, deformation of the joint space, appearance of bone spines and growths. |
| Basic treatment | Anti-inflammatories | Chondroprotectors |
A similar feature of both diseases is a progressive course with a gradual loss of mobility. Autoimmune arthritis often manifests itself at a young age, when a person is still frivolous about their health.
It should be remembered that any joint pain that lasts a long time occurs under certain conditions; this is a serious reason to see a doctor. It is important to diagnose the disease in time and start its treatment in order to slow down the development of the pathological process.



































